Strengthening health systems for resilient communities
Well-functioning health systems are essential for fostering resilient communities capable of responding and recovering from significant shocks. Communities that prioritise preparedness, collaboration, and knowledge-sharing are more resilient, and can mitigate the impact of health crises on livelihoods, societies, and economies. Enhancing public health system capacities must remain a priority, including in EU cooperation with partner countries.
Recent crises have redefined the European health agenda, highlighting the importance of health for well-being and stability. Health is both a core sector of humanitarian aid and a main reference for measuring a humanitarian response. In fragile settings, whether characterised by sudden emergencies or protracted crises, healthcare services can be heavily disrupted. Last month, DG ECHO updated its policy guidelines on Health Response in Humanitarian Settings to improve health preparedness and better health outcomes for affected people.
National Red Cross and Red Crescent Societies, supported by the International Federation of Red Cross and Red Crescent Societies (IFRC), work with communities around the world to prevent, prepare for, and respond to health threats and public health emergencies, such as epidemics and pandemics. Through their auxiliary role, staff and volunteers work with local people, public authorities and other health sector partners to ensure inclusive access to high quality health services, including in hard-to-reach and remote areas.
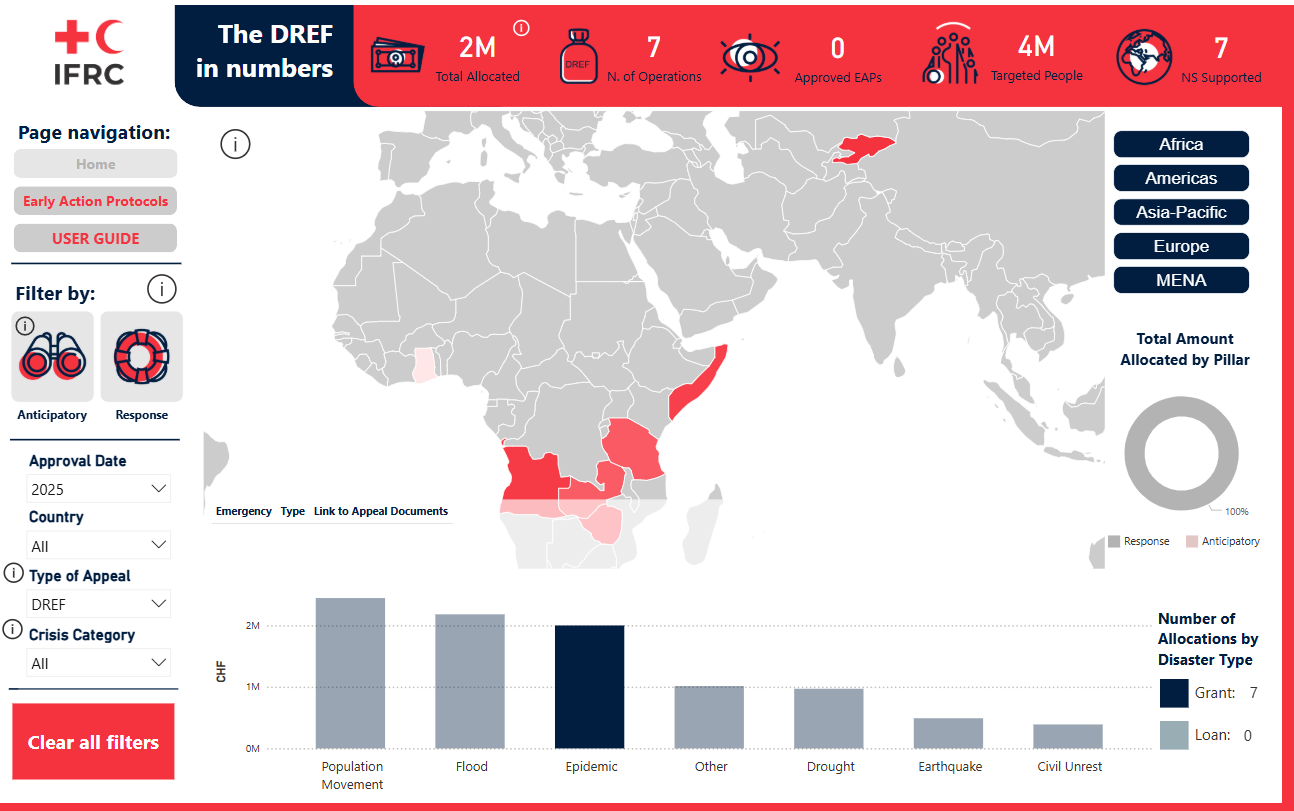
For example, in the first months of 2025 alone, the IFRC network has responded to epidemic outbreaks through seven Disaster Response Emergency Fund (DREF) operations, including with the support of DG ECHO. Based on this expertise, we contributed to the consultation launched by DG ECHO to revise these important policy guidelines. We stressed the importance of meaningfully engaging local actors, of strengthening the health care “work force”, including volunteers, and of reflecting the links between climate and health – recommendations that we are pleased to see reflected in the final document.
The primary responsibility for capacity development in response to health crises lies with national public health authorities. However, epidemics begin and end in communities, making the involvement of local actors and affected communities essential to protect people and ensure that their humanitarian needs are effectively addressed. The policy guidelines recognise this by promoting activities like risk communication and community-based surveillance (CBS). By equipping people with the skills and tools to quickly report unusual health events, CBS helps make sure the right help is provided in the right place and at the right time to prevent epidemics or reduce their harm.
For example, Kyrgyzstan Red Crescent volunteers in Talas have been trained to recognise signs of common diseases and report unusual animal deaths. “If volunteers see something unusual whilst out conducting risk communication activities within their communities, they send an SMS alert to their supervisor. Then the case is reported to the nearest medical or veterinary centre, at which point a doctor or veterinarian comes out to investigate,” explains Gulnura Abdumanapova, Kyrgyzstan Red Crescent Health Coordinator.

Importantly, the policy guidelines have widened the definition of “workforce”, including community health workers, volunteers, and “other allied health professionals who play a role in preventing, diagnosing, treating, and caring for people, including those who do not deliver services directly but are essential to the performance of health systems.” Training and equipping them to respond to emergencies while ensuring a safe, secure and healthy work environment are key. The guidelines also emphasise health system sustainability and preparedness to ensure continuity for access to healthcare, including diagnosis and treatment, for people with chronic diseases and non-communicable diseases (NCDs).
Finally, the cascading impacts of climate crisis present immense challenges for human health. Access to safe, clean water remains fundamental as it directly influences key health determinants such as nutrition, hygiene, and disease prevention. Also, climate change and lack of drinking water directly hampers health delivery. This is especially true for people living in marginalised communities, particularly in complex emergency situations, as they are more affected by gaps in accessing drinking water and sanitation. Health emergency responses must always be carried out in line with the humanitarian principles and without stigma and discrimination.
These guidelines advance the EU’s commitment to protect health across all policies. In order to do so, equitable partnerships that reach the people experiencing heightened vulnerabilities is essential. Strengthening coordination, effectiveness, and accountability among public, private and civil society actors and donors at all levels is the way forward.
For media inquiries, please contact Eva Oyón on: eva.oyon@redcross.eu or +32 2 235 09 22

